Some of the best recent science has shown us that there may be common causes underlying the complex symptoms of Gulf War veterans’ illnesses, and those causes very likely involve the brain and neurological system.
Among the scientific studies that I have found to be particularly compelling have been those that suggest that various Gulf War exposures led to subtle brain and nervous system damage in Gulf War veterans, which, in turn, has led to dysfunctions of the autonomic nervous system, that controls such “automatic” bodily functions as the heart rate, breathing, digestion, salivation, perspiration, sexual functioning, and sleep regulation.
In short, many scientists now believe that Gulf War Illness is its own separately diagnosable condition, distinct from MS and lupus and even from nearby cousins fibromyalgia, chronic fatigue syndrome, and irritable bowel syndrome. Others still disagree. However, what’s important is that many scientists have found neurological symptoms in ill Gulf War veterans than can be treated and even if not completely reversed, at least mediated and made more bearable.
Recognizing Gulf War Illness as a separate and distinct neurological condition, caused by chemical damage to the brain and resulting in diverse neurological, autonomic nervous system, and immunological symptoms, is by far the most plausible and most comprehensive explanation I have seen in all the years I’ve been active on Gulf War illness issues.
This article is divided into four parts after this introduction, including the probable damage caused by certain Gulf War exposures, neurological tests and symptoms, what works, and what to avoid.
Because this article is already so long, I plan to cover sleep, stress management, deep breathing, digestion and gut issues later in separate columns. Your comments below this article are always welcome, particularly those about your own experiences of what works and what doesn’t.
----------------------------------------------------------
Part 1: Acetylcholine, Gulf War Exposures, and Brain Damage. I have found it to be of particular interest and plausibility in these theories that a brain and nervous system chemical called acetylcholine, a primary transmitter of nerve impulses in the autonomic nervous system, was and continues to be affected by one or more common Gulf War exposures.
 Remember the little white pills so many of us Gulf War veterans took after the war began, the ones that we were told were experimental and unapproved by the FDA but which we were required to take anyway? Those Pyridostigmine Bromide (PB) pills we Gulf War veterans took were sometimes also called Nerve Agent Protective Pills, or NAPP’s. The primary purpose of constantly taking PB during the Gulf War was to disrupt the production of acetylcholine and improve our chances of survival after a nerve agent attack when used in combination with our 2-PAM chloride and atropine injectors that we carried everywhere as part of our basic uniform, right along with our protective gas masks.
Remember the little white pills so many of us Gulf War veterans took after the war began, the ones that we were told were experimental and unapproved by the FDA but which we were required to take anyway? Those Pyridostigmine Bromide (PB) pills we Gulf War veterans took were sometimes also called Nerve Agent Protective Pills, or NAPP’s. The primary purpose of constantly taking PB during the Gulf War was to disrupt the production of acetylcholine and improve our chances of survival after a nerve agent attack when used in combination with our 2-PAM chloride and atropine injectors that we carried everywhere as part of our basic uniform, right along with our protective gas masks.
However, without even discussing the long-term effects, taking the PB pills had immediate negative effects on many of us, and so much so that we remember them 20 years later. In my own hastily unit of 35 or so guys that constituted our hastily pulled together liaison team, roughly two-thirds or so of us showed or talked about negative side effects we were having from the PB pills while we were taking them, which we were told would mimic mild effects of nerve agent poisoning and which they did. Among those effects were: Runny nose; Watery eyes; vision changes; drooling and excessive sweating; cough; chest tightness; more rapid breathing; diarrhea; confusion; drowsiness and fatigue; weakness; headache; nausea, vomiting, and abdominal pain. Some of us had all the symptoms, some only a few, some were affected badly with substantial weight loss and being laid up on bed rest while others were affected only a little.
Meanwhile, a number of important scientific studies since the Gulf War have helped unravel the short- and long-term effects of PB pills, both alone and when taken in combination with being exposed to the military-strength pesticides that were so common among Gulf War troops.  Those pesticides we Gulf War troops used as protection against sand flies, mosquitoes, and other biting insects, included permethrin, which was supposed to be sprayed on our uniforms to saturate them with insecticide but which we sometimes sprayed right onto our bodies as wells as our tents, sleeping bags, mosquito netting, and in our vehicles.
Those pesticides we Gulf War troops used as protection against sand flies, mosquitoes, and other biting insects, included permethrin, which was supposed to be sprayed on our uniforms to saturate them with insecticide but which we sometimes sprayed right onto our bodies as wells as our tents, sleeping bags, mosquito netting, and in our vehicles.  It also included DEET, a commonly used insect repellant contained in “Off” insect sprays but which we Gulf War troops used in incredibly high concentrations all the time. Recent research has shown DEET to be an inhibitor of the key brain chemical acetylcholinesterase even on its own.
It also included DEET, a commonly used insect repellant contained in “Off” insect sprays but which we Gulf War troops used in incredibly high concentrations all the time. Recent research has shown DEET to be an inhibitor of the key brain chemical acetylcholinesterase even on its own.
And, at least one scientific study has shown that while PB pills might improve survivability after an attack using Soman, one of the more common chemical warfare agents in the Gulf War era Iraqi arsenal, the use of PB actually heightens the negative health effects of Sarin, another common Iraqi chemical warfare agent to which an estimated 100,000 U.S. troops were exposed at low levels following the post-war demolition of chemical and other munitions at an Iraqi weapons storage depot at Khamisiyah, Iraq in March 1991. Soman, Sarin, and a close cousin of Sarin called Cyclosarin all also negatively impact the brain and nervous system, including affecting the production and reception of acetylcholine in the autonomic nervous system.
What is also significant is the result of studies that have shown that while PB does not normally cross the brain-blood barrier, stress can allow it to cross over into the brain with short- and long-term effects that are only in the early stages of being discovered.
To show how seriously many in the scientific research world are now taking this PB and PB-pesticide connection to Gulf War veterans’ illnesses, a 2008 U.S. government report by the Congressionally-chartered Research Advisory Committee on Gulf War Veterans’ Illnesses shook the scientific world when it identified PB-pesticides as the leading probable cause for most Gulf War veterans’ chronic multi-symptom illness – though the report did not rule out a number of other hazardous exposures as having caused other conditions prevalent or potentially prevalent among Gulf War veterans. The panel is composed of some of the top scientists in their fields from the U.S. and UK, including a former elected head of the American Association for the Advancement of Science, the head of neuro-toxicology for the U.S. Centers for Disease Control (CDC), the head of the UK’s center for chemical warfare research, and many others. In short, these are not scientific lightweights, off-beats, or self-serving quacks by any stretch of the imagination -- which have all too often been the scourge of the Gulf War veteran community. The collective opinion of these leading scientists, rooted in countless scientific studies, represented a true and major breakthrough for Gulf War veterans suffering from Gulf War Illness.
Of interest to Gulf War era troops who did not deploy, these highly concentrated pesticides have more recently been shown to be dangerous were used commonly throughout the military at the time. This fact might help explain why some non-deployed Gulf War ere troops report long-term symptoms similar to some Gulf War veterans.
The damage caused by these acetylcholinesterase inhibiting agents is only just beginning to be understood by science. I’m most encouraged by many of the scientists involved who suggest that this new understanding may very well lead to treatments that might help.
----------------------------------------------------------
Part 2: Neurological tests and Symptoms. Meanwhile, here are some of the neurological effects I’ve experienced since the Gulf War, whatever the cause, that are common to many of us Gulf War veterans.
· Chronic, debilitating fatigue. This was one of the earliest symptoms, which began while I was still in the Gulf and was first taking the PB pills. However, we had a lot of exposures during the Gulf so accurately attributing the overwhelming fatigue to any one or any set of them is difficult. Chronic Fatigue Syndrome (CFS) is another presumptive condition for Gulf War veterans. Like so many other Gulf War veterans, the fatigue is overwhelming to the point of being all-encompassing and is impossible to overcome. Fatigue is difficult to measure, but there are a number of fatigue scales that can be used. Some scientists and medical doctors believe that the chronic, debilitating fatigue in Gulf War Illness is separate and distinct from CFS, and a number of current studies will try to tease that distinction out as part of their various aims. And in the last year, a virus called XMRV has been identified in people with CFS which might be the cause of their chronic fatigue symptoms. If any of this turns out to be true, then treatment for Gulf War veterans might be the same or different than for those with CFS.
· Chronic muscle and joint weakness. This has been getting progressively worse over time. After the Gulf War, even though I was only in my early- to mid-20’s, I began experiencing my knees and legs just giving out. Muscle and joint weakness are commonly reported symptom among Gulf War veterans with chronic multi-symptom illness, as well as in veterans in general, and this is one area that’s harder to tease out from the long-term symptoms of excessive wear and tear on our joints and muscles from our military experiences. Over time, I’ve had more and more difficulty with walking, a commonly reported neurological or arthritis-based complaint among many Gulf War veterans.
· Chronic widespread pain. In many Gulf War veterans, our chronic widespread pain has been given the diagnosis of Fibromyalgia, which is a presumptive condition for service-connection for us Gulf War veterans. For me, this is in the muscles, tendons, joints, and spine. Fibromyalgia has traditionally been diagnosed through a pressure-point diagnosis system that is still being used by the VA in its diagnostic tests for determining service-connection. However, a newer system is being used in some areas that involves a pain index along with measuring other fibromyalgia syndrome symptoms like fatigue, cognitive symptoms, and psychological symptoms.
Like with CFS, some scientists and medical doctors believe that the chronic widespread pain in Gulf War Illness is separate and distinct from fibromyalgia, and a number of current studies will try to tease that distinction out as part of their various aims. If this is true, then treatment for Gulf War veterans’ chronic widespread pain might be different than for those with fibromyalgia. Time will tell in these scientific debates.
· Paresthesias/Dysthesias. These classic neurological symptoms involve unpleasant, painful, or other highly unnatural-feeling sensations in the skin and various parts of the body. For me, they range from buzzing and unpleasant tingly/buzzing feelings, feelings of vibration, pinching and needle-poking symptoms, to small, repeated twitching. At its worst, they feel like deep burning hot, freezing cold, and a feeling of the affected area being unpleasantly wet – all impossibly at the same time.
While other ill Gulf War veterans have told me about getting these in virtually every part of the body, for me, my Paresthesias are most often in my feet and legs. In my legs, it starts off as tingling, buzzing, and twitching that becomes increasingly painful. I also often get aching feet that quickly progresses to burning and feeling like I’m stepping on hundreds of sharp nail points. I often get paresthesias up and down my spine and neck, which begin as strong tingling and progress to pain, sometimes they even go up over the top of my head. One of the strangest feelings is when I get these inside the right side of my abdomen, where it feels exactly like my cell phone is vibrating, only it goes on for minutes or hours. These sensations feel very abnormal, and are often very difficult to describe.
Some Gulf War veterans have told me about getting these neurological symptoms even in their face and eyes. In my case, my doctors attribute these classic neurological symptoms to fibromyalgia and Gulf War Illness, though they’re also common symptoms in Multiple Sclerosis (MS), Lupus, neurological damage caused by Diabetes, and a host of other neurological diseases. Very little study has been devoted to Paresthesias/dysthesias in Gulf War veterans, though my own experience suggests that this is more of a newly emerging issue in us Gulf War veterans and part of the progression of the underlying issues, and hopefully we’ll see more treatment-focused research aimed in this direction in the next year or two.
· Neuropathies. These are nerve-related pain. For me, I get them most in my legs and feet, sometimes with Paresthesias/dysthesias, sometimes alone, but I know other Gulf War veterans that get them in their hands, arms, face, and elsewhere. Neuropathy is common in MS, Lupus, Diabetes, and many other neurological diseases. My father is a diabetic who gets neuropathies in his legs that are so severe he cannot sleep, and this is also reportedly common among Gulf War veterans.
· Comprehensive neurological testing. I found it very important to have a complete battery of comprehensive neurological testing to rule out other neurological diseases. These included an Electromyogram and nerve-conduction studies (EMG/NCS), a battery of in-office basic neurological tests, an MRI of the brain, an EEG, neuropsychiatric tests to measure memory, cognitive abilities, mood and emotional dysfunctions, and many others. Read more these and neurological testing here: http://www.ninds.nih.gov/disorders/misc/diagnostic_tests.htm
a complete battery of comprehensive neurological testing to rule out other neurological diseases. These included an Electromyogram and nerve-conduction studies (EMG/NCS), a battery of in-office basic neurological tests, an MRI of the brain, an EEG, neuropsychiatric tests to measure memory, cognitive abilities, mood and emotional dysfunctions, and many others. Read more these and neurological testing here: http://www.ninds.nih.gov/disorders/misc/diagnostic_tests.htm
· Small Fiber Peripheral Neuropathy (SFPN). Many of the standard neurological tests are looking at neurological symptoms and conditions in the most broad-brush sort of way. I know a lot of Gulf War veterans who have grown upset over the years because a neurologist has not been able to diagnose or find a cause for the apparently neurological symptoms they’re reporting. A new study is currently focusing on the possibility of a condition called Small Fiber Peripheral Neuropathy in Gulf War veterans with Gulf War Illness symptoms, which cannot be diagnosed by the older, more traditional neurological tests like EMG’s and NCS’s because they’re simply not sophisticated enough. If SFPN is found to be an issue, this could quickly lead to new treatment possibilities for Gulf War veterans. Typical symptoms include burning feet and numb toes.
· Vision changes. While I have only had limited vision symptoms, many of my ill Gulf War veteran friends report eye pain, double vision, blurred vision, and other color and vision changes that wax and wane. Some of these Gulf War veterans have been diagnosed with MS, while others have not.
· Dizziness. This is a commonly reported symptom among Gulf War veterans. It’s also very hard to diagnose or measure. This is also a common symptom in veterans with mild and other Traumatic Brain Injury (TBI) caused by head injuries, blast waves, and other concussions. It’s important for a good doctor to do a thorough review, including a detailed medical history that includes when the dizziness began, because dizziness can be a symptom with many possible causes, some of them life-threatening. Most important is whether the dizziness waxes and wanes, stays the same, or has been getting progressively worse with no relief.
· Heat Intolerance. Like people with MS, I’m a Gulf War veteran without MS who has developed heat intolerance. Just like people with MS, heat – including from a hot day, a hot shower or bath, a hot tub or sauna, or even a hot kitchen – makes my other symptoms flare almost instantly, including fatigue, weakness, dizziness, cognitive issues and visual symptoms.
· Headaches. I’ve been fortunate to not have headaches, a common symptom reported by many Gulf War veterans, since my sinus surgeries in the mid-1990s. I sometimes wonder how many of my fellow Gulf War veterans’ headaches could be attributed to untreated and possibly unknown sinus problems as well. At least one Gulf War Illness researcher continues to look at migraines in Gulf War veterans.
· Brain/Spinal Cord lesions. Many Gulf War veterans have told me about having had lesions found on their brain and/or spinal cord after an MRI. Some are diagnosed with MS, while others are not. Some have told me that their doctors call the lesions atypical for MS and are unexplained. There has been a good bit of discussion among ill Gulf War veterans about deterioration of the myelin sheath surrounding nerves as a possible cause for some of Gulf War veterans’ neurological symptoms, similar to the dramatic demyelination in MS.
· CSF changes. Certain changes in the cerebral-spinal fluid (CSF) that surrounds the brain and spinal cord are used to confirm the diagnosis of MS and other neurological diseases. A sample of CSF is drawn via a spinal tap. Many studies have found an increase of a particular chemical believe to be related to pain sensation, called Substance P, in the CSF of people with Fibromyalgia.
For me, I have unusually high protein levels in my CSF, which is consistent with my neurological symptoms, but doesn’t really help to guide any specific form of treatment, at least not yet, anyways. A study currently ongoing at Georgetown University in Washington, DC may help shed more light on abnormalities in ill Gulf War veterans’ CSF and has the potential of helping to provide another objective diagnostic criteria that might also one day be used to measure the severity or progression of the underlying issues.
· Blood Abnormalities. Some neurological diseases show certain abnormalities that can be identified by specific testing of blood samples. Neurology and Immunology can both help in these areas, though getting more exotic testing done can be difficult to impossible within the VA system due to budget and formulary constraints.
· Cognitive issues. These were some of the earliest symptoms reported by ill Gulf War veterans, including memory loss, confusion, excessive or even debilitating forgetfulness, decreased ability to learn or retain information, difficulties with words and speaking, new onset difficulties with reading, and other related cognitive issues. Like many Gulf War veterans, I’ve experienced many of these, too. These issues are also common symptoms of PTSD, a common war trauma disorder, and mild and other Traumatic Brain Injury (TBI and mTBI).
· Mood Issues. Symptoms like depression and anxiety are common in many debilitating diseases, but especially in brain and neurological disorders. Mood swings, excessive irritability, and mental lethargy can also be symptoms. Many of these are also symptoms in PTSD, which affects many veterans, and in TBI/mTBI, another form of brain injury. Effective treatment of these is critical, though working with a doctor to find medications that work and also have tolerable side effects can be a challenge spanning several years.
While some veterans I know are concerned about the supposed stigma of being seen or treated for these issues, it should come as no surprise to anyone thatp people with neurological damage of any kind are at increased risk of also having mood symptoms, since most mood controls reside in the brain and neurological system that in many Gulf War veterans is likely damaged.
· Sexual Function Issues. Much of the body’s sexual functioning is controlled by the parts of the brain believed to be damaged in Gulf War veterans. Sexual function can also be negatively impacted by other forms of brain injury, and by PTSD, depression, and anxiety, all of which are prevalent in military veterans. Issues related to the several aspects of sexual function are an important but little discussed aspect of Gulf War Illness, the impact of which obviously differs between male and female Gulf War veterans. For many Gulf War veterans and their families, these symptoms have had a profound impact on conception, and childbearing, relationship health, and quality of life. In the early years after the Gulf War, “burning semen syndrome” and birth defects were two areas that were widely discussed and derided in the stress-bent military establishment, but there was little serious scientific or medical attention given to these issues. Despite the highly private and sensitive nature of these issues, perhaps the future will hold more focused research targeted to these areas.
----------------------------------------------------------
Part 3: Neurological Symptoms -- Things that help. Here are some of the things I do that seem to help my own neurological symptoms.
· Sleep. Getting good quality sleep for Gulf War veterans, particularly for those of us also suffering from PTSD, can be nearly impossible, and I intend to dedicate a column just on sleep alone. In summary, however, a combination of sleep hygiene techniques, deep breathing exercises discussed below, stress management (also to be the subject of another column), sleep medications, and control of sleep apnea symptoms are all key.
· Medications. There are many medication choices for neurological pain and neurological symptoms like Paresthesias/dysthesias, neuropathies, and other neurological symptoms. These range from drugs like Lyrica, which is specifically approved to fibromyalgia pain and in my experience really does help relieve the worst Paresthesias, to narcotics and opiods like oxycodone, oxycontin, vicodin and other medication specifically for pain.
As surprising as what it might seem, some anti-depressants, anti-seizure medication used in conditions like epilepsy, muscle relaxants, and anti-anxiety mediations can be helpful in treating the wide array of neurological symptoms and underlying issues.
While I have never tried Amitriptyline (Elavil) this is another commonly prescribed first-line drug for neuropathic pain. I’ve heard mixed reports from other Gulf War veterans and fibromyalgia sufferers, helping some and not helping others. It’s often necessary for VA doctors to try prescribing these sorts of drugs first before progressing to more expensive drugs like Lyrica if the first- and second-line drugs don’t work.
Gabapentin (Neurontin) is an anti-seizure drug that is often prescribed for neuropathic pain, especially if amytriptaline isn’t effective. I found it did not relieve my paresthesias, though it did help with the neuropathies.
Lyrica (Pregabalin) is the general favorite of four drugs now FDA-approved for the treatment of fibromyalgia. While Gabapentin works on the brain’s GABA-receptors, Pregabalin, like the names sounds, works at a level prior to that.
Other FDA-approved drugs for fibromyalgia include Cymbalta (Duloxetine) and Savella (milnacipran), two drugs which cannot be taken in combination with some other anti-depressant type medications. Cymbalta is also FDA-approved for treating depression and diabetic peripheral neuropathy.
I’ve also found that analgesics like prescription strength Ibuprofen (Motrin) helps with some of the muscle pain (but not the nerve pain). For me, I have found a combination of these helpful, though I personally try to avoid narcotics and opioids. However, that’s a very personal choice made based on my own weighing of the Faustian trade-offs of leaving the symptoms untreated versus experiencing the unavoidable side-effects of those types of medications. Many other Gulf War veterans need to rely heavily on these kinds of pain medications. In fact, pretty much all neurological drugs are going to have side-effects, some of which may be worse than the symptom you’re trying to have treated.
I have found neurology and rheumatology to be most helpful in diagnosing and treating my own pain, Paresthesias/dysthesias, and other neurological issues.
Here’s a really good PowerPoint overview of neurological drugs: http://cstl-hhs.semo.edu/ham/ns270-01/protected/NS%20270%20Neurologic%20Drugs.ppt
Modafanil (Provigil) is commonly prescribed for fatigue issues. I don’t like it, just like I don’t like caffeine, because they both make me work past my fatigue limits and lead to sever flare-ups in my pain and other symptoms, but others’ experiences may be different, of course.
· Treatments for cognitive symptoms vary from psychological adaptation and learning to do things differently to sort of “bypass” the damaged areas of the brain, to medications, neutraceuticals and supplements, to strategies and tools to help with memory like a smart phone (iPhone, Blackberry, etc.) or personal digital assistant (PDA, like Palm Pilots, iPods, iPads, etc.). It’s important to learn that no matter what the cause is for brain damage, we’re very resilient and can do a lot to adapt. While it’s hard, we can learn new ways of doing things to help us get by, much like an amputee gets by with a new prosthetic limb.
I rely on my smart phone for sounding off to remind me of things I need to do, and my iPad for my calendar and daybook that also beeps and makes other sounds to let me know of upcoming appointments and other scheduled activities. Having a family member keep track of appointments is also helpful, and something that we do in my family so I don’t miss them.
· Cognitive support. In addition to reading and writing to keep my mind active, I really like Ginkgo Biloba, an over the counter neutraceutical herbal supplement that seems to have only one effect – improving my mental clarity – with no apparent side effects. I take two standard capsules every morning as part of my daily regimen, and while the improvement is subtle, it is noticeable. I order mine online at less than $3/bottle: http://www.swansonvitamins.com/mobile/itemdetail/SW1106.html.
· Treatment for Mood Issues. Common symptoms in neurological and other diseases, like depression and anxiety, mood swings, excessive irritability, and mental lethargy, need to be treated. Effective treatment of these is critical, though working with a doctor to find medications that work and also have tolerable side effects can be a challenge spanning several years. There is no shame in getting this kind of treatment, any more than there is any shame in getting pain medication for pain, heart medication for heart disease, or inhalers for lung and sinus disease. And, as I already noted above, many of these treatments are also known to affect pain receptors in the brain and are specifically prescribed to reduce pain and other neurological symptoms, meaning multiple benefits in the same treatment!
For example, Celexa (Citalopram) has been shown to be effective in relieving symptoms of depression, PTSD, and is also prescribed off-label for chronic widespread pain. I’ve had good success with it.
· Exercise, even moderate, helps the chronic widespread pain. However, for me and many other Gulf War veterans, this is sort of a Catch-22 because the exercise also often dramatically worsens the debilitating fatigue. A powerful recent study showed that Tai Chi helps with managing chronic fibromyalgia pain.
· Walking Support. A lot of Gulf War veterans I know have difficultly with mobility. Some have been diagnosed with MS, while most of the rest of us have not. While it can be a bit of a pride issue, using the cane prescribed by my doctor really does help with mobility and in countering the gradually progressing weakness in my legs and back. Add in the degenerative arthritic issues in my knees and spinal column, and having walking support is critical. Using a shopping cart for support when in large stores is also very helpful. While I spent the better part of a year at Walter Reed Army Medical Center recovering from a non-combat military injury leg surgery, I learned that it’s most effective to use a cane on the opposite side of the weakest one, and having the can high enough so you can stand straight up without leaning are both key.
· Deep Breathing. I’ll do a separate article on this one, but if you want to get a head starte, here’s a good article on deep breathing exercises: http://www.drweil.com/drw/u/ART00521/three-breathing-exercises.html
· Stress Management. Just the word “stress” has become a trigger point and dirty word for many Gulf War veterans because of the federal government’s insistence over many of the early years after the Gulf War that “all” that was wrong with Gulf War veterans was “stress” -- and that we just needed to forget about it, get over it, and get past it. (One VA doctor, my local VA Gulf War specialist, actually told me and other Gulf War veterans those words in 1996). However, managing stress and our reactions to it is a key part of dealing with any serious and debilitating disease like Gulf War Illness, fibromyalgia, chronic fatigue syndrome, MS, and so on. I plan a separate column on stress management for ill Gulf War veterans, including its importance and some “how-to’s”.
· Laying flat on your back. Strange as it may sound, this can really help with quelling the worst of the symptoms. Sometimes, even sitting up can make symptoms worse. Laying flat on my back, or laying flat with my knees up, really seems to help. I’ve found the real versatility of a laptop, and in fact, I’m writing this from my laptop while flat on my back. I don’t know whether this helps anyone else, or if anyone else can feel a difference from sitting up versus laying down, but it works for me so maybe it works for someone else, too.
----------------------------------------------------------
Part 4: Neurological Symptoms and Things to avoid. Here are some of the things I avoid in order to not make my neurological symptoms worse, or keep the worst of them at bay.
- · Head and Neck Injuries. I’ve found that many of my symptoms have dramatically worsened each time I’ve had an additional head or neck injury. While probably no one really tries to get a head or neck injury, avoiding situations that put you at higher risk might be a good choice.
- · Avoid certain chemicals. Like many Gulf War veterans, I became highly chemically sensitive while still in the Gulf. From paints and paint thinners to pesticides, detergents, and almost any sort of chemical fume, I’ve learned to avoid them to prevent immediate worsening of my symptoms. I’m interested in what others have learned to avoid – put it as a comment below!
- · Avoid certain food additives. I’ve found that caffeine makes me worse even in very small amounts (a few sips of coffee or a caffeinated soda), which like for everyone first boosts my energy, but then crashing down into a serious and debilitating fatigue episode that can last as long as 24 hours or more. I also avoid aspartame (Nutrasweet), found in diet sodas, powdered diet drinks, chewing gum, and many other products, since it has made me feel unpleasantly light-headed in even very small quantities. By paying attention to how I feel after I consume anything, this helps.
- · Overexertion. For me, balancing has been key. A balance between a little moderate exercise (a walk of a few blocks, walking while doing some light shopping) and getting a LOT of rest is critical.
- · Stress. I can’t say enough about how important it has been, especially in more recent years, to keep all stress away to keep the worst of the symptoms at bay. This includes both physical strain and mental or emotional stress.
- · Driving. I have found that the constant, subtle jostling while driving or riding in a car makes my neurological symptoms worse. Flying isn’t quite as bad. In addition to becoming highly fatigue, sometimes even short, in-town driving/riding can bring on the worst of the neurological symptoms.


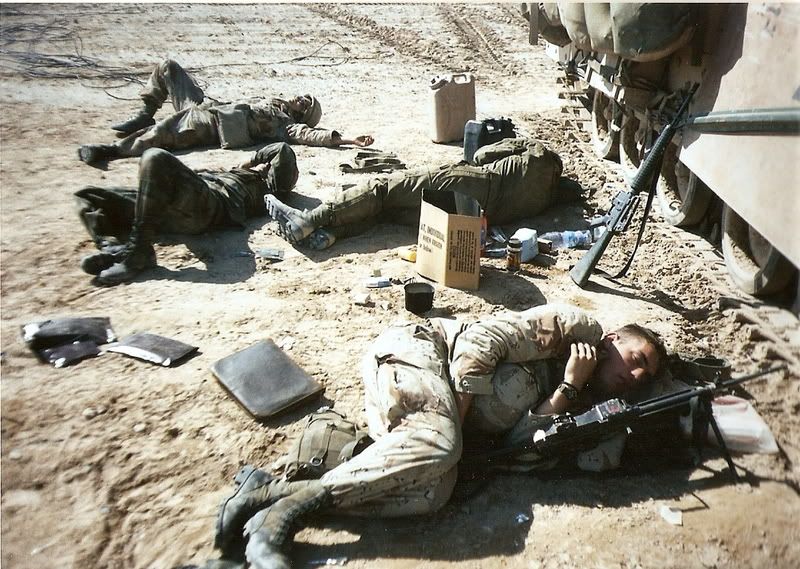 iecing together sleep throughout a 24-hour or longer period; learning to sleep with one eye (or ear) open to remain watchful for the enemy; never getting a full night’s sleep; waking up for guard duty or other night-time tasks, then having to go back to sleep for an hour, two, or three afterwards; overuse of caffeine and other stimulants; performing all daily tasks like eating, reading, watching a DVD, cleaning your weapon on the same cot, bunk, mat, or vehicle where you sleep because it’s the only home you have. But in order to correct these and other issues, first, you need to know what to do.
iecing together sleep throughout a 24-hour or longer period; learning to sleep with one eye (or ear) open to remain watchful for the enemy; never getting a full night’s sleep; waking up for guard duty or other night-time tasks, then having to go back to sleep for an hour, two, or three afterwards; overuse of caffeine and other stimulants; performing all daily tasks like eating, reading, watching a DVD, cleaning your weapon on the same cot, bunk, mat, or vehicle where you sleep because it’s the only home you have. But in order to correct these and other issues, first, you need to know what to do. CPAP. A machine to help in breathing while sleeping, called a
CPAP. A machine to help in breathing while sleeping, called a 
 Those pesticides we Gulf War troops used as protection against sand flies, mosquitoes, and other biting insects, included permethrin, which was supposed to be sprayed on our uniforms to saturate them with insecticide but which we sometimes sprayed right onto our bodies as wells as our tents, sleeping bags, mosquito netting, and in our vehicles.
Those pesticides we Gulf War troops used as protection against sand flies, mosquitoes, and other biting insects, included permethrin, which was supposed to be sprayed on our uniforms to saturate them with insecticide but which we sometimes sprayed right onto our bodies as wells as our tents, sleeping bags, mosquito netting, and in our vehicles.  It also included DEET, a commonly used insect repellant contained in “Off” insect sprays but which we Gulf War troops used in incredibly high concentrations all the time. Recent
It also included DEET, a commonly used insect repellant contained in “Off” insect sprays but which we Gulf War troops used in incredibly high concentrations all the time. Recent  a complete battery of comprehensive neurological testing to rule out other neurological diseases. These included an
a complete battery of comprehensive neurological testing to rule out other neurological diseases. These included an