
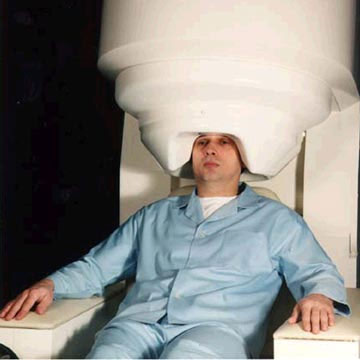
Ft. Hood Accused Shooter, U.S. Army Maj. Nidal Hasan
By Daniel Zwerdling, January 21, 2010
(NPR) - The Army has told some of the psychiatrists who supervised Fort Hood shooting suspect Nidal Hasan that it’s investigating them — and they could face punishments from letters of reprimand to court martial.
The Army said it’s going to decide if the doctors at Walter Reed “failed to take appropriate action” against Hasan and were “derelict” in their duties.
Evidence shows a lot of doctors were worried about Hasan — some for years. Evidence also shows that only one supervisor, Scott Moran, actively tried to kick Hasan out of the psychiatry program. Now sources involved in the investigation say Moran is one of the officers who’s in big trouble. Moran wouldn’t comment, but the sources say the supervisors under investigation are fairly low level officers like Moran, who is a major.
“They’re attacking the wrong target,” says Gary Myers, a lawyer who’s representing Col. Charles Engel, another psychiatrist whom Myers says is under investigation.
Engel was Hasan’s main supervisor in the fellowship program at the military’s medical school, the Uniformed Services University of the Health Sciences. Myers says the Army is trying to find scapegoats and that everybody knows officials in the nation’s intelligence agencies bear at least some responsibility for what happened at Fort Hood.
Read entire article: http://www.npr.org/templates/story/story.php?storyId=122778372
==========================
Military Doctors Worried Hasan Was 'Psychotic,' Capable of Killing Fellow Soldiers
Published November 12, 2009
(FoxNews.com) - U.S. military doctors overseeing Nidal Malik Hasan's medical training were concerned he was "psychotic" and possibly capable of killing other American soldiers, before the Army major allegedly went on a deadly shooting rampage at Fort Hood, Texas.
Psychiatrists and medical officials at Walter Reed Army Medical Center held a series of meetings beginning in the Spring of 2008 to discuss serious concerns about his work and behavior, National Public Radio reported.
One of the questions they asked: Was Hasan psychotic?
"Put it this way," one official told NPR. "Everybody felt that if you were deployed to Iraq or Afghanistan, you would not want Nidal Hasan in your foxhole."
One official who participated in the discussions reportedly told others he was worried that if Hasan was deployed to Iraq or Afghanistan, he might leak covert military information to Islamic extremists, NPR reported.Another official "wondered aloud" to colleagues whether Hasan might be capable of killing fellow soldiers in the same way a Muslim sergeant in 2003 had set off grenades at a base in Kuwait, killing two and wounding 14, the radio network reported.
The officials who discussed Hasan's status were unaware — as some top Walter Reed hospital officials were — that intelligence agencies had been tracking Hasan's e-mails to a radical imam since December 2008, NPR said.
Officials considered kicking Hasan out of the program but chose not to partly because firing a doctor is a "cumbersome and lengthy" process that involves hearings and potential legal conflict, sources told NPR.
Officials also believed they lacked solid evidence that Hasan was unstable and were concerned they could be accused of discriminating against him because of his Islamic identity or views.
The concerns about Hasan's performance and religious views were shared with other military officials considering his assignment after he finished his medical training, and the consensus was to send the 39-year-old psychiatrist to Fort Hood, an official told the Associated Press.
Hasan was characterized in the meetings as a mediocre student and lazy worker, a matter of concern among the doctors and staff at Walter Reed and the Uniformed Services University of the Health Sciences, a military medical school in Bethesda, Maryland, an official told The Associated Press.
Fort Hood, one of the country's largest military installations, was considered the best assignment for Hasan because other doctors could handle the workload if he continued to perform poorly and his superiors could document any continued behavior problems, the official said.
Sharon Willis, a spokeswoman for the Uniformed Services University, referred questions Wednesday about Hasan to his lawyer. The attorney, John Galligan of Belton, Texas, did not immediately return a telephone call seeking comment.
The revelations about the concerns that Hasan's superiors had before sending him to Fort Hood come amid a growing debate over what warning signs the military and law enforcement officials might have missed before last week's massacre.
A joint terrorism task force overseen by the FBI learned late last year of Hasan's repeated contact with a radical Muslim cleric who encouraged Muslims to kill U.S. troops in Iraq. The FBI said in a statement late Wednesday that the task force did not refer early information about Hasan to superiors because it concluded he wasn't linked to terrorism.
The doctors and staff who discussed concerns about Hasan had several group conversations about him that started in early 2008 during regular monthly meetings and ended as he was finishing a fellowship in disaster and preventive psychology this summer, the official familiar with the discussions said.
They saw no signs of mental problems, no risk factors that would predict violent behavior. And the group discussed other factors that suggested Hasan would continue to thrive in the military, factors that mitigated their concerns, the official said.
According to the official, records reviewed by Hasan's superiors described nearly 20 years of military service, including nearly eight years as an enlisted soldier; completion of three rigorous medical school programs, albeit as a student the group characterized in their discussions as mediocre; his resilience after the deaths of his parents early in his medical education, and an otherwise polite and gentle nature when not discussing religion.
The Army has said it has no record of enlisted service for Hasan, instead noting that his military service began when he started the medical school program in 1997.
The official said the group became increasingly concerned about Hasan's religious views after he completed two research projects that took a decidedly religious tone — one at the end of his residency at Walter Reed that advocated allowing Muslim soldiers to be released as conscientious objectors instead of fighting in wars against other Muslims, and the other as he pursued his master's degree in public health that discussed religious conflicts for Muslim U.S. soldiers.
Some in the group shared their experiences with Hasan, all telling similar stories about repeated instances when he made religion an issue.
Officials involved at various times in the meetings about Hasan included John Bradley, Walter Reed's chief of psychiatry; Scott Moran, Walter Reed's psychiatric residency program director; Robert Ursano, chairman of the Uniformed Services University's psychiatry department; Charles Engel, the university's assistant chair of psychiatry, and David Benedek, an associate professor of psychiatry at the university.
Those officials either declined to comment or did not return telephone calls and e-mails seeking comment Wednesday.
Meanwhile, the Pentagon has found no evidence that Hasan formally sought release from the Army as a conscientious objector or for any other reason, two senior military officials told The Associated Press. Family members have said he wanted to get out of the Army and had sought legal advice, suggesting that Hasan's anxiety as a Muslim over his pending deployment overseas might have been a factor in the deadly rampage.
Hasan had complained privately to colleagues that he was harassed for his religion and that he wanted to get out of the Army. But there is no record of Hasan filing a complaint with his chain of command regarding any harassment he may have suffered for being Muslim or any record of him formally seeking release from the military, the officials told the AP.
The officials spoke on condition of anonymity because the case is under investigation.
Another Army official, Lt. Col. George Wright, said Wednesday that Hasan likely would have had to commit to another year in the military when he was transferred to Fort Hood earlier this summer. It is common for an officer to incur a one-year service extension when they receive a transfer to another post.
The Associated Press contributed to this report.
=========================================
January 21, 2010 Thursday
DEPARTMENT DEFENSE BRIEFING
NATIONAL PUBLIC RADIO "MORNING EDITION" REPORT;
SUBJECT: "ARMY DOCTORS COULD FACE DISCIPLINE IN FORT HOOD CASE" REPORTERS: RENEE MONTAGNE, DANIEL ZWERDLING
NATIONAL PUBLIC RADIO "MORNING EDITION" REPORT SUBJECT: "ARMY DOCTORS COULD FACE DISCIPLINE IN FORT HOOD CASE" REPORTERS: RENEE MONTAGNE, DANIEL ZWERDLING TIME: 7:15 A.M. EST DATE: THURSDAY, JANUARY 21, 2010
MS. MONTAGNE: Returning to the story of Nadal Hasan, the U.S. Army major charged in last year's Fort Hood shooting. NPR has learned the Army has told some of the psychiatrists supervising Hasan at Walter Reed Hospital that it's investigating them and they may face punishment. The Army said it will decide whether the doctors, quote, "failed to take appropriate action against Hasan and were derelict in their duties."
One name on the list of supervisors is a surprise as NPR's Daniel Zwerdling reports.
MR. ZWERDLING: The evidence shows that a lot of doctors were worried about Nadal Hasan for years. The evidence also shows that only one supervisor actively tried to kick Hasan out of the psychiatry program, his name is Scott Moran. So here's the surprise. Sources involved in the investigation say that Scott Moran is one of the officers who is now in big trouble.
Moran wouldn't comment, but the sources tell NPR that all the supervisors under investigation are fairly low level officers like Moran. He's a major.
GARY MYERS: They're attacking the wrong target.
MR. ZWERDLING: Gary Myers is a lawyer who is representing another psychiatrist whom he acknowledges is under investigation. His client is Colonel Charles Engel. Engel was Hasan's main supervisor in the fellowship program at the military's medical school. Meyers says the Army is trying to find scapegoats. He says everybody knows by now that officials in the nation's intelligence agencies bear at least some responsibility for what happened at Fort Hood.
MR. MEYERS: The notion that that it is attributable to lower level physicians who were also mentors strikes me as being a bullet fired high and to the right.
MR. ZWERDLING: A spokesman for the Army said they won't confirm or deny that they've notified any officers that they're under investigation. As you might remember, NPR reported troubling details about Hasan's medical career back in November. We reported that right after Scott Moran took over the psychiatrist residents program back in March 2007, he reviewed Hasan's record and he told colleagues they should get rid of him. Moran wrote a memo to the powerful credentials committee. The memo denounced Hasan for a pattern of poor judgment and a lack of professionalism. But sources and documents confirm that higher ups told Moran to back off. They said going after Hasan might cause legal hassles.
Next, Hasan went to a fellowship at the military's medical university and documents show that supervisors there got upset, too. Some of Hasan's supervisors were concerned that Hasan seemed to have extremist Islamist beliefs. Hasan seemed obsessed with a Muslim American soldier who killed fellow troops in Kuwait. Some supervisors even wondered out loud, could Nadal Hasan be psychotic?
Sources say the Army is investigating Charles Engel because he knew about those concerns, yet he allegedly didn't take tough enough action. Those same sources say the Army is investigating another psychiatrist named Colonel John Bradley for the same reason. Bradley has been running the psychiatry department at Walter Reed and colleagues say both men kept telling them, we're running training programs here, we're supposed to help people like Hasan try to improve. And sources say when they got on his back, Hasan occasionally did better work.
The investigation of Scott Moran is more puzzling since documents suggest that he's the only one who actively tried to go after Hasan. Documents show that Moran did sign paperwork later that recommended Hasan for promotion, but that was after higher ups rebuffed him. So far, there's no sign that the Army is investigating those higher ups.
NPR tried to reach Moran, Bradley and Engel for comments. None of them responded. Sources say the Army has notified several other mid-level officers that they're being investigated, too. The Army won't confirm those details either.
Daniel Zwerdling, NPR News.
January 21, 2010
===========================================
COL Charles Engel, M.D., M.P.H., mentioned in the press accounts above, currently serves on the Congressionally Directed Medical Research Program’s (CDMRP) Gulf War Illness Research Program (GWIRP) FY2010 Integration Panel.







 Navigating fibro
Navigating fibro Not tracking your pain
Not tracking your pain Expecting too much from medication
Expecting too much from medication Refusing to consider off-label drugs
Refusing to consider off-label drugs Not exploring alternatives
Not exploring alternatives Sticking with the wrong doctor
Sticking with the wrong doctor Denying that you’re sick
Denying that you’re sick Not enlisting family support
Not enlisting family support Not reaching out to others
Not reaching out to others Not talking about it
Not talking about it Feeling guilty
Feeling guilty Letting fibromyalgia get to you
Letting fibromyalgia get to you Taking life too seriously
Taking life too seriously Not moving because it hurts too much
Not moving because it hurts too much

